Basic Wound Care Principles
Basic Principles of Wound Care:
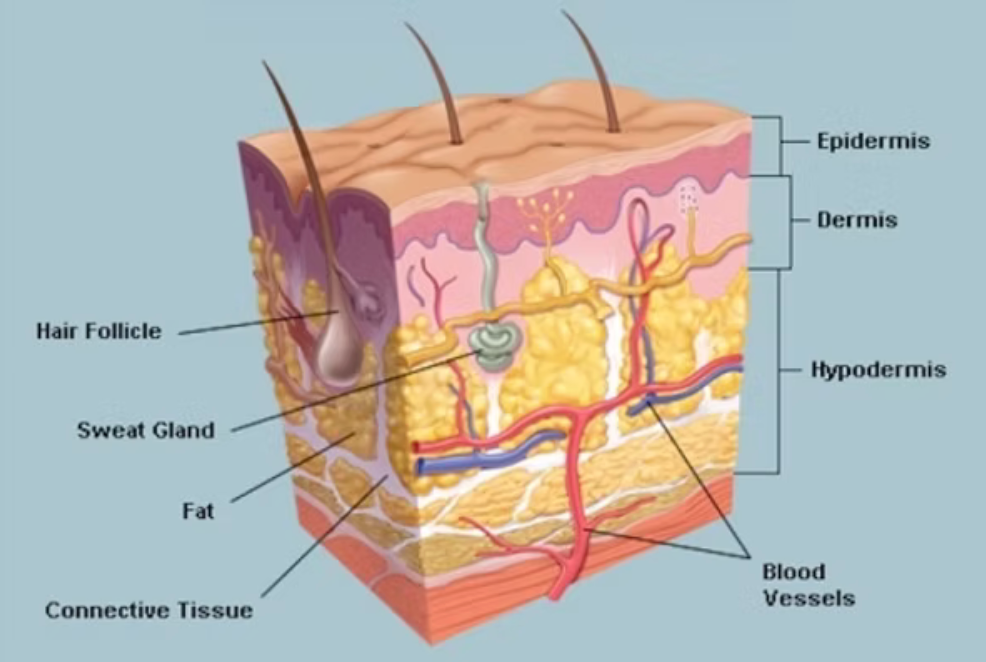
A wound can be described as a disturbance of the normal anatomical relationship between body tissues and is generally accompanied by a break in the skin. As soon as a wound occurs, the skin and its components become actively involved in the wound healing process to restore the integrity of the skin as soon as possible and to ensure its protective function. The depth classification or grading of pressure soars, burns, and leg ulcers is assessed by determining which skin structures and/or underlying tissues have been penetrated or damaged.
The skin as an organ:
The skin is one of the largest and one of the most important organs of the body, considering the variety of functions it performs. This organ is often damaged because of its direct contact with the external environment. Skin damage includes injuries such as bruises, abrasions, and stab wounds; exposure to nature’s elements, such as sunburn; and exposure to chemicals. An adult’s skin surface area is approximately 1,2 - 2,0 m2 and compromises approximately 16-17% - one-sixth of total body weight. Under normal circumstances, it receives approximately 33% of the circulating blood volume. It has a PH of 5.5 (slightly acid), which affords the skin certain protective properties. Only normal skin flora flourishes in the acid environment of intact skin and together with the acid environment inhibits the proliferation and colonization of pathogenic micro-organisms. As an organ, the skin is a combination of various tissue types that carry out complex and specific functions in collaboration and mutual interaction with one another. All four primary tissue types- epithelium, connective, muscle, and neural – occur in the skin.
Dermis:
This is the second main layer of the skin, also known as the corium. It is a compact connective tissue layer of about 3.0 mm in thick and 0.5mm in thinner skin. The basal membrane firmly joins the epidermis and dermis, and the connection is known as the dermal-epidermal junction. Blood and lymph vessels and nerves are found in this layer. It is generally accepted that the blood supply is primarily for the regulation of temperature and blood pressure, and secondly for the nutrition of the skin.
The connective tissue consists of large amounts of collagen (protein), elastic, and reticular fibers. They also migrate to damaged or injured areas to assist the recovery process.
Macrophages (white blood cells) also have the ability to migrate out of the circulation to the dermis and to move about there in the
matrix, also known as the ground substance (gelatine-like inter-cellular fluid in tissue). They penetrate inflamed, damaged, or injured tissue with the aim of clearing up damaged or dead tissue and toxic substances.
Mast cells are large cells that are also found in the connective tissue of the dermis. When a wound occurs, they secrete histamine at the start of the inflammatory phase of wound healing.
Fibroblasts, macrophages, and mast cells play a role in wound healing.
The matrix is of great physiological value as it contains important components such as proteins, mucopolysaccharides, fluid collagen, immune bodies, and metabolites.
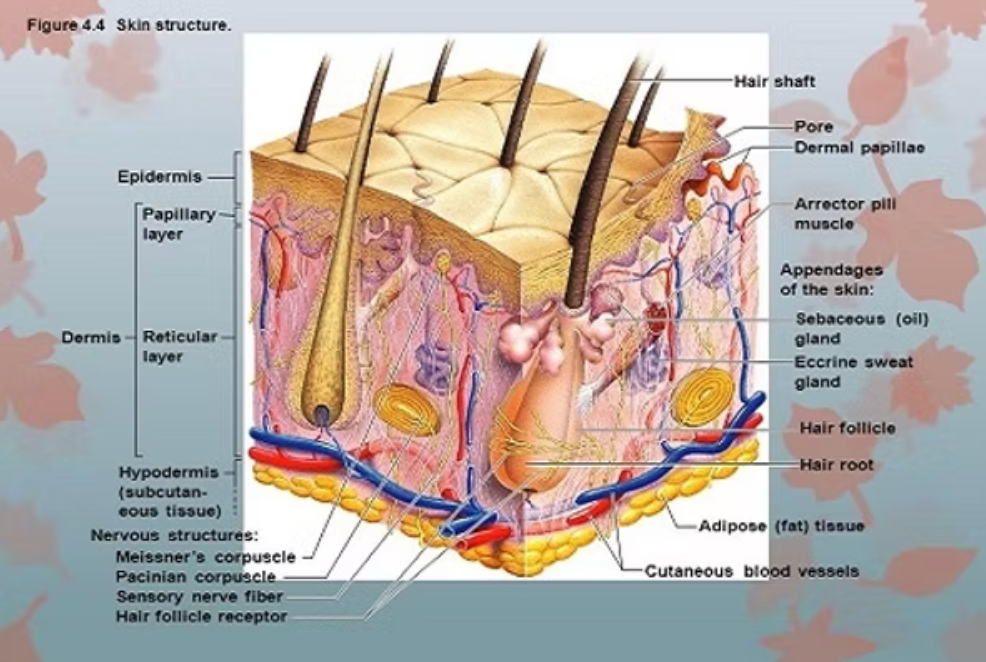
The Dermis is divided into two layers:
- Papillary layer
- Reticular layer
1. The papillary layer:
- This layer is characterized by dermal evaginations or papillae that extend to between the epidermal ridges.
- Encapsulated sensory nerves of touch and temperature and open nerve endings for pain are situated in this layer
- Partial and second-degree burns extend into this layer.
2. The reticular layer:
- Reticular means “like net” but the connective tissue in this layer is compact.
- Bundles of collagen fibers extend into this layer.
- The collagen fibers extend also into the subcutaneous layer, to ensure the Dermis is rigidly attached to the rest of the body
- Partial-thickness/second-degree burns extend into this layer.
The Subcutaneous layer
- This is a layer of loose connective tissue that supports the skin and attaches to the underlying structures such as muscles, bone, and organs.
- It also supports the larger blood vessels, lymphatic vessels, and the nerves that branch to the dermis
- Wounds such as the full thickness of third-degree burns, pressure sores, and leg ulcers extend into this layer.
LOCAL FACTORS:
Local factors that influence the rate of healing include impaired blood supply; temperature fluctuations; the wound site; local infections; foreign bodies; necrotic tissue; slough and eschar, desiccation; pressure, fracture and shear, changes in oxygen tension; skin maceration; and
topical applications.
Impaired blood flow:
- Disturbances to the peripheral blood supply will reduce tissue perfusion, limiting the local supply of oxygen and other nutrients required for tissue repair.
Temperature fluctuations:
- A fall of 2% at the wound interface is enough to reduce the rate of oxy-hemoglobin dissociation and oxygen availability, inhibiting cell division significantly and slowly the formation of new tissue. Research has found that a constant temperature of 37 C promotes both the macrophages and mitotic activity during granulation and epithelialization. Temperature extremes also cause tissue damage.
Wound Site:
- The position of a wound affects its vascularity and determines the mobility of the wound site. Wounds on, or close to joints tend to heal slower as the constant movement may disrupt the delicate, new tissue.
Local infection
- All chronic wounds, such as pressure sores, contain bacteria. However, there is no evidence to suggest that bacteria need to be removed from chronic wounds for healing to occur.
- Chronic wounds are typically seen in the elderly, and the immune response may be absent. The most obvious sign of wound infection is that it will not start healing. This is because wound infection prolongs the inflammatory phase, causes further tissue damage, and delays collagen synthesis and epithelialization.
Foreign bodies, necrotic tissue, slough, and eschar
The presence of necrotic tissue, slough, and eschar wound healing by impeding epithelial migration and impairing the supply of nutrients to the wound bed. It may act as a medium for bacterial growth and subsequent infection. Foreign bodies, such as cotton wool fibers, can cause tissue irritation, prolong the inflammatory response, and act as foci for infection.
Pressure, friction, and shear
Mechanical forces, such as pressure, friction, and shear, significantly impair wound healing by prolonging tissue damage. These forces are discussed in chapter 17.
Skin Maceration
If the surrounding wound area is exposed to excess moisture from exudate, perspiration or incontinence, maceration, and damage to the surrounding skin can occur. This may predispose to infection, skin sensitivities, irritation, further skin breakdown, and impede wound healing.
Reason for moist healing:
Winter (1962) compared healing in dry and moist superficial wounds and found that the moist wounds formed new epidermal covering 40% faster than the dry wounds. The same author concluded that this was because new epidermal cells could migrate easily across the moist wounds, whereas in the dry wound, the cells had to negotiate the scab, which took longer. Subsequent research suggests that the inflammatory process is accelerated in a moist environment, leading to faster healing. Conversely, a dry environment will lead to dehydration and cell death.
Psychosocial assessment and management.
The presence of a wound, particularly a chronic wound, can cause stress, anxiety, and depression in a patient.
- Calm patient
- Give hope
- Relief pain
- Take photos to see improvement
- The correct ointment
Wounds are classified according to their depth or the tissue layers that are damaged or destroyed.
- Erosion involves the loss of one or two layers of epithelial cells. There is no depth to this type of wound.
- Superficial wounds occur where the epidermis has been damaged.
- A partial-thickness wound is one where the epithelium and part of the dermis are destroyed. Hair follicles and sweat glands are only partially damaged. This type of wound is sometimes subdivided into partial-thickness and deep partial-thickness wounds.
- Full-thickness wounds involve the destruction of all the epidermis, and dermis, subcutaneous tissue, and possibly muscle and bone.
Factors influencing wound healing
1.
Nutrition
Several macro and micro-nutrients play a role in the wound-healing process.
2.
Protein
Protein, a fundamental requirement in the healing process assists in neo-vascularisation, fibroblast proliferation, collagen synthesis, lymph formation, and wound remodeling. It is also associated with collagen and proteo-glycan synthesis. Protein deficiency decreases the body’s resistance to infection as it alters antibody response time and leucocyte capabilities. The inflammatory process is prolonged and fibroplasia impaired. Collagen synthesis is also impaired, and macrophage production is decreased. An indicator for visceral protein status = is to do serum albumin levels = hypo-albumin a (<32g/l) promotes * GENERELISED OEDEMA THAT SLOWS OXYGEN DIFFUSION AND METABOLIC TRANSPORT MECHANISMS FROM THE CAPILLARIES AND CELL MEMBRANE.
3.
Carbohydrates
It is needed for cellular energy and is associated with collagen and proteo-glycan synthesis.
4.
Fats
Fat (fatty acids), as a source of cellular energy, is required for the normal functioning of cell membranes and promotes cell synthesis. A deficiency of this nutrient may inhibit tissue repair.
5.
Water
Water constitutes 65-70-% of total body weight and is the medium in which most metabolic processes occur. Water is considered the most important nutrient and essential to life. Loss of water or dehydration results in electrolyte imbalance, impaired cellular function, and, therefore, delayed wound healing.
Micro-nutrients
- Vit A – Vit A is a co-factor in collagen synthesis and cross-linkage. It is essential for the stimulation of fibroplasia and epithelialization. Vit A deficiency leads to altered collagen synthesis and cross-linking between fibers, this results in a decreased rate of epithelialization in wound closure.
- Vit B Complex – contributes to antibody and white cell formation; is a co-factor in cellular development and promotes enzyme activity necessary for the metabolism of proteins, fats, and carbohydrates. Deficiency results in decreased resistance to infection.
- Vit C – Vitamin C is a co-factor for the enzyme collagen prolyl hydroxylase. This is used in the formation of the triple helix of collagen. Vit C is essential for neutrophil superoxide production and bacterial killing.
- Vit E – Has an important protective role in antioxidant defense and wound healing.
- Vit K – Plays an essential role in coagulation.
- Iron – is vital to red cell function because it enables the transport of oxygen.
- Zinc- is a critical element in protein synthesis and tissue repair.
Collagen:
Collagen is the main structural protein in the extracellular space in the various connective tissues. As the main connective tissue, it is the most abundant tissue, making 25% to 35% of the whole-body protein content. Collagen consists of amino acids to form triple helices and elongated fibrils. It is mostly found in fibrous tissues such as tendons, ligaments, and skin. Collagen is one of the body’s key natural resources and a component of skin tissue that can benefit all stages of the wound healing process. Collagenase can be made by the body as part of its normal immune response.
Studies have shown:
Incisional wounds:
The highest collagenase activity was observed on post-op day 1 and then it decreases. Beyond day 10 no activity was detected. Granulation tissue from non- sutured large full-thickness wounds, showed high collagenase content on postoperative day 5 and then a sharp decline today 7 followed by a slowly declining curve to postoperative day 21. Activity on day 5 was threefold the activity on day seven.
Partial-thickness
wounds exhibited a different time course, with collagenase increasing from day 1 to days 3-5. By day 7 collagenase concentrations approached the low concentrations of normal skin when epithelialization was complete.
USING ILOSUN OINTMENT DURING THE INFLAMMATORY FASE WHEN COLLAGEN LEVELS IS HIGHER AFTER INJURY, THE RESULTS ARE REMARKABLE. WHEN ILOSUN OINTMENT AND “BODY” WORK TOGETHER DURING THIS PHASE. RAPID HEALING TAKES PLACE WITHOUT SCAR FORMATION OR DELAYED HEALING PROCESSES WHICH CAN LEAD TO OVER GRANULATION AND SKIN GRAFTS. ALLWAYS AIM TOWARDS EARLY REPAIR.
Surrounding Skin
Little attention has been given to the need to care for the skin around the wound. The skin surrounding the wound may be intact, erythematous, indurated, oedematous, fragile, dry-scaling, or macerated.
Intact, healthy skin is vulnerable to:
- maceration
- erosion
- insults from wound exudate,
- repeated dressing changes
- or other trauma,
And therefore needs to be protected.
Wound exudate may aggravate peri-wound skin damage, either directly or by injuring the surrounding skin (excoriation), and delayed healing may provoke local irritation or allergic reactions. (contact dermatitis)
Photographic methods:
The simplest non-contact technique is that of photography. To monitor the progress of healing by taking photographs, it is
- Essential that each photograph is comparable to the others.
- To achieve such consistency, it is necessary to exercise as much control as possible over the variables that may influence the results.
- Each view should be matched for size, view, point, and framing
- Use the same camera or cell phone for each wound trial
- Must be a color photo
- Patient position in relation to the camera with each photo. Notes can be made of position and distance from the camera for every photo
- The amount, angle, and direction of LIGHT FALLING on the subject must be controlled. May the same room, positioning, and time.
- The background should be plain and unobtrusive. No bright light in the background.
- Maintain the same distance every time (not to close)
- Written consent from the client/patient to take photos.
- Important: Wound studies should be done by a responsible person who is well educated in using Ilosun Ointment. No harsh methods of cleaning. Gentle wound healing.
More Posts Like This



